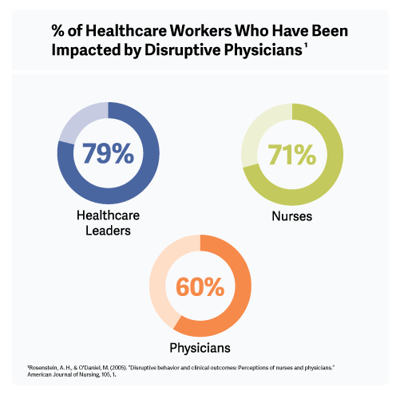
When a physician engages in disruptive behavior, defined by the AMA as “verbal or nonverbal conduct that harms or intimidates others to the extent that quality of care or patient safety could be compromised,” the ripple effect of the behavior can be extreme and the results quite dire, according to studies.1
Nurse retention
In a 2005 study, nurses called disruptive behavior the single most important contributing factor to lowered job satisfaction and morale and 31% said they knew at least one nurse who left because of it. Given the cost of replacing a nurse can be from 1.5 to 2 times his or her annual salary, the bottom-line impact of disruption is a serious concern.2
Patient safety
According to a 2003 survey by the Institute for Safe Medication Practices, 49% of clinicians have felt pressured by an intimidating physician to dispense or administer a drug despite their serious objections based on safety concerns. In fact, 40% have kept quiet rather than question the intimidator.3 In a 4,530-participant survey conducted at 102 VA hospitals, 67% of the respondents said they felt disruptive behavior was linked to adverse events, 71% saw a link to medical errors and 27% saw a link between disruption and patient mortality.4
Patient and family dissatisfaction
A 2011 review of complaints to state medical boards from patients and family members showed 36% of them were related to inappropriate behavior by physicians.5
The evidence, then, is clear. Disruptive behavior by physicians is no longer “par for the course,” a regrettable but natural aspect of medicine’s authority structure, but rather a hazard to be understood and worked against for the benefit of everyone involved in medicine.
To adequately address disruption, leadership needs to take three crucial steps, according to the research and recommendations of employment attorney Judith Holmes and healthcare-business consultant Leigh Olson, in an article for the Medical Group Management Association.6 The three leadership steps include:
Confront the problem: Let staff know the administration takes the problem seriously, the incident is not
“business as usual.”
Enlist help: Working with at least one other physician, set a meeting with the disrupter; allow them to explain
their understanding of the incident; tell them a performance improvement plan is being drafted, to which they
will be strictly held.
Develop a prevention plan: A set of policies and protocols on behavior that all must follow.
For details on dealing with disruption, see our article “How to Successfully Manage the Obstacles of a
Disruptive Physician.”
Visit our Physician Intervention page for additional resources and information. Contact VITAL WorkLife by visiting us online.