Physicians choose to end their own lives at about twice the rate of the general population1 and experience higher suicide rates than those serving in the military2. It’s clear health care organizations need to be concerned about the conditions which may lead to suicidal ideation among their practitioners and do what they can to alleviate those conditions. Suicide is a complex and often daunting issue with multiple contributing factors, from unnoticed/undiagnosed depression and substance abuse to personal problems related to finances, health, or family. Another significant contributor can be burnout—the loss of self-belief and the sense of making a difference that can afflict physicians stressed by the escalating demands of contemporary medical practice. Organizations need to take steps to understand the relationship between burnout and suicide, and an important place to start is with the attitudes and experiences of physicians themselves.
To this end, in 2018 Medscape surveyed some 15,000 American practitioners across 29 specialties. The Medscape National Physician Depression, Burnout, and Suicide Report 20193 tallied their responses and pointed up some significant realities:
Burnout, which the study defined as “long-term, unresolvable job stress that leads to exhaustion and feeling overwhelmed, cynical, detached from the job, and lacking a sense of personal accomplishment,” is a significant problem. Forty-four percent of respondents considered themselves to be suffering from it.
- But physicians resist getting help. Sixty-four percent of respondents said they do not plan to seek professional help for burnout, and have not sought such help in the past.
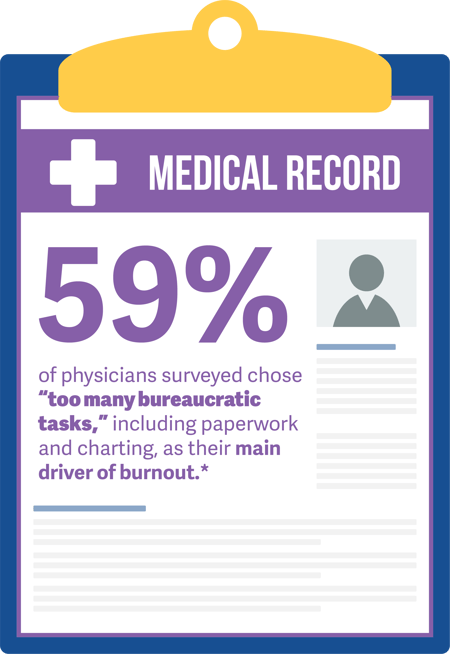
- By a large margin (59 percent), the physicians surveyed chose “too many bureaucratic tasks,” including paperwork and charting, as the main driver of burnout, followed by “spending too many hours at work” (34 percent) and “increasing computerization of practice” (32 percent).
- More than an eighth of the respondents (14 percent) reported they had considered suicide, but had not acted on these thoughts. One percent said they had attempted suicide.
- Practitioners are hesitant to open up to other practitioners about this issue. Sixty-seven percent of those who had considered suicide shared the thoughts with a therapist or a family member, but only 23 percent confided in a medical colleague.
There are other important lessons to be learned from the survey, but these five are enough to underline the need for organizations to ask themselves whether they have a workplace culture which promotes physician well-being, openness about problems, and mutual support.
VITAL WorkLife offers proactive and preventive solutions designed to support physicians and organizations align collaboratively. Contact us online to learn more about our services.
For more on physician suicide and measures which can head it off, see our Article "Healing the Healer: Providing a Path Towards Physician Suicide Prevention."*"The Medscape National Physician Depression, Burnout, and Suicide Report 2019." Medscape, 2019