Early-career practitioners are at particular risk for burnout. A 2018 Mayo study, for example, found 45 percent of residents surveyed had experienced at least one warning sign.1 Organizations wanting to retain and nurture young medical talent need to be proactive against the phenomenon—and one initiative in the Bay Area is showing what can work: mentoring and social support, along with knowledge about best practices for supporting well being.
The Neurology Wellness and Mentoring Program, started in 2018 by two young neurologists at Stanford Medical, supports students, fellows and faculty in the specialty by emphasizing human connections. Besides creating mentorship relationships between senior and younger doctors, the program connects practitioners through lunch conferences and social “teams” based not on medical specialties but on outside interests and commonalities, like parenting and running.2
Breaking Isolation
The program doesn’t address certain major drivers of burnout, including intense performance metrics and the challenges of electronic health records, but it does focus on breaking the isolation which can afflict physicians in demanding environments. And the lunch sessions treat resilience-related topics such as sleep, practicing gratitude, nutrition and how to have difficult conversations.
Measurable Results
The results of the program’s first year have been encouraging: when participants self-assessed on the Personal Fulfillment Index questionnaire, they reported a decrease in feelings of interpersonal disengagement after four months—and the decrease was sustained at 10 months. They noted a gradual increase in the sense of professional fulfillment which became significant after 10 months. And they felt a decrease in burnout and an increase in “compassionate self-improvement” at both time points.
“We want to make wellness a legitimate concern, something that is okay to talk about,” Rebecca Miller-Kuhlmann, MD, one of the program’s originators, tells Neurology Today. “We want to normalize that burnout is an issue, that we need to support each other, and this is something that we need to be doing.”
“Support each other” seems to be the operative phrase here: burnout recedes when physicians are in compassionate connection with one another.
For more on early-career burnout and how to handle it, see our article “The Challenges of Well Being: Battling Early Career Physician Burnout.”
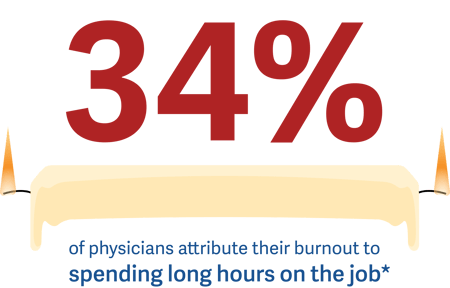
*"Physician burnout in 2019, charted," Advisory Board, January 18, 2019